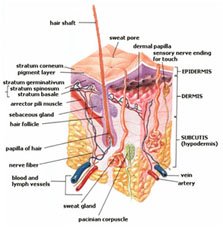
It starts when greasy secretions from the skin's sebaceous glands plug the tiny openings for hair follicles (plugged pores). If the openings are large, the clogs take the form of blackheads: small, flat spots with centers darkened by exposure to air. If the openings stay small, the clogs take the form of whiteheads: small, closed, flesh-colored bumps. Both types of plugged pores can develop into swollen, tender inflammations or pimples or deeper lumps or nodules. Cysts associated with severe cases of acne (cystic acne) are firm swellings below the skin's surface that become inflamed and sometimes infected.
Although acne remains largely a curse of adolescence, about 20% of all cases occur in adults. Acne commonly starts during puberty between the ages of 10 and 13 and tends to be worse in people with oily skin. Teenage acne usually lasts for five to 10 years, normally going away during the early 20s. It occurs in both sexes, although teenage boys tend to have the most severe cases. Women are more likely than men to have mild to moderate forms into their 30s and beyond.
Acne lesions are most common on the face, but they can also occur on the neck, chest, back, shoulders, scalp, and upper arms.
Acne isn't caused by a harmful diet, poor hygiene, or an uncontrolled sex drive. The simple truth is that heredity and hormones are behind most forms of acne. Swearing off chocolate or scrubbing your face 10 times a day won't change your predisposition to this unsightly, sometimes painful, and often embarrassing skin problem.
The Causes
The cause of acne is not fully understood. Though poor hygiene, poor diet, and stress can aggravate acne, they clearly do not cause it.
Hormones.
Common acne in teenagers starts with an increase in hormone production. During puberty, both boys and girls produce high levels of androgens, the male sex hormones that include testosterone. Testosterone signals the body to make more sebum, a waxy substance that helps the skin retain moisture. Androgens also boost the production of keratin, a substance used by the body to make hair and nails.
Bacteria.
Excess sebum clogs the openings to hair follicles -- especially those on the face, neck, chest, and back. Bacteria grow in these clogged follicles. This makes blackheads or whiteheads form on the skin's surface -- a condition called non-inflammatory acne. Sometimes the follicle wall breaks under the pressure of this buildup. When this happens, sebum leaks into nearby tissues and forms a pustule -- this is called inflammatory acne. This can create cysts. Ruptured cysts leave temporary or permanent scars.
Depending on the type of pill, oral contraceptives may trigger acne in some women but suppress it in others. Steroids taken by some bodybuilders and other athletes can also lead to severe outbreaks.
Acne has many subtypes. Acne neonatorum and acne infantum occasionally affect newborns and infants, usually boys. A pimply rash appears on the face but usually clears within weeks with no lasting effect. People who escaped their teen years almost pimple free may develop persistent adult-onset acne as they get older. Despite the normal increase in androgen levels during puberty, some doctors believe that flare-ups of acne have less to do with androgen levels than with how a person's skin responds to an increase in sebum production. The bacteria Propionibacterium acnes and Staphylococcus epidermidis occur naturally in healthy hair follicles. If too many of them accumulate in plugged follicles, they may secrete enzymes that break down sebum and cause inflammation. Some people are simply more sensitive than others to this reaction. Sebum levels that might cause a pimple or two in one person may result in widespread outbreaks -- or even acute cystic acne -- in another person.
Risk factors
Hormonal changes in your body can provoke or aggravate acne. Such changes are common in:
- Teenagers, both in boys and girls
- Women and girls, two to seven days before their periods
- Pregnant women
- People using certain medications, including cortisone
Other risk factors include:
- Direct skin exposure to greasy or oily substances, or to certain cosmetics
- A family history of acne — if your parents had acne, you're likely to develop it too
- Friction or pressure on your skin caused by items such as telephones or cell phones, helmets, tight collars and backpacks
- Foods - it is still to be a controversy about food inducing acnes. It is a very individual reason, when chocolate, nuts, milk or other fatty foods and even eggs can induce acne in several people.
How does acne happen?
There are oil glands on your chest, face and back numbering in the thousands. In fact, between the nose and cheek areas there are as many as two thousand oil glands every square inch. The function of these oil glands is to lubricate the skin by producing oil, or sebum. Oil that is produced in the glands flows through follicles or tiny ducts to the surface of the skin. It usually starts far beneath the surface of the skin. A blemish (or internal lump) begins about 2 to 3 weeks before it appears on your skin's surface. Acne first begins to form in your sebaceous hair follicles. You know this as "pores", the tiny holes on you skin. Deep within each hair follicle, sebaceous glands generate sebum, the oil that keeps your skin soft, moist and pliable. As part of your skin's renewal process the old cells die and are shed off. Normally, this cell shedding process happens gradually, and fresh new skin takes its place.
But sloughing (the process where living tissue is separated from dead skin tissue) is not the same for everyone. Some people shed cells evenly while others don't. The result of uneven sloughing is that dead cells become sticky, clogging together to form a plug, similar to a cork in a bottle. This plug traps oil and bacteria inside the follicle.
The trapped oil begins to form a lump as your skin continues its normal oil production. Your body's natural defense system then sends an army of white blood cells to attack the bacteria. The whole process takes around 2 to 3 weeks, resulting in a pimple.

Acne typically appears on your face, neck, chest, back and shoulders, which are the areas of your skin with the largest number of functional oil glands. Acne can take the following forms:
- Comedones (whiteheads and blackheads). Comedones (kom-uh-DO-neze) are created when the openings of hair follicles become clogged and blocked with oil secretions, dead skin cells and sometimes bacteria. When comedones are open at the skin surface they're called blackheads because of the dark appearance of the plugs in the hair follicles. When comedones are closed, they're called whiteheads — slightly raised, skin-colored bumps.
- Papules. These are small raised bumps that signal inflammation or infection in the hair follicles. Papules may be red and tender.
- Pustules. Similar to papules, pustules are red, tender bumps with white pus at their tips.
- Nodules. These are large, solid, painful lumps beneath the surface of the skin. They're formed by the buildup of secretions deep within hair follicles.
- Cysts. These are painful, pus-filled lumps beneath the surface of the skin. These boil-like infections can cause scars.





Acne usually isn't a serious medical condition. But you may want to seek medical treatment from a dermatologist for persistent pimples or inflamed cysts to avoid scarring or other damage to your skin. If acne or the scars it may have left are affecting your social relationships or self-esteem, you may also want to ask a dermatologist if your acne can be controlled or if your scars can be diminished.
Treatment
Acne treatments work by reducing oil production, speeding up skin cell turnover, fighting bacterial infection, reducing the inflammation or doing all four. With most prescription acne treatments, you may not see results for four to eight weeks, and your skin may get worse before it gets better.
Your doctor or dermatologist may recommend a prescription medication you apply to your skin (topical medication) or take by mouth (oral medication). Oral prescription medications for acne should not be used during pregnancy, especially during the first trimester.
Types of acne treatments include:
- Topical treatments. Acne lotions may dry up the oil, kill bacteria and promote sloughing of dead skin cells. Over-the-counter lotions are generally mild and contain benzoyl peroxide, sulfur, resorcinol, salicylic acid or lactic acid as their active ingredient. These products can be helpful for very mild acne. If your acne doesn't respond to these treatments, you may want to see a doctor or dermatologist to get a stronger prescription lotion. Tretinoin (Avita, Retin-A, Renova) and adapalene (Differin) are examples of topical prescription products derived from vitamin A. They work by promoting cell turnover and preventing plugging of the hair follicles. A number of topical antibiotics also are available. They work by killing excess skin bacteria. Often, a combination of such products is required to achieve optimal results.
- Antibiotics. For moderate to severe acne, prescription oral antibiotics may be needed to reduce bacteria and fight inflammation. You may need to take these antibiotics for months, and you may need to use them in combination with topical products.
- Isotretinoin. For deep cysts, antibiotics may not be enough. Isotretinoin (Accutane) is a powerful medication available for scarring cystic acne or acne that doesn't respond to other treatments. This medicine is reserved for the most severe forms of acne. It's very effective, but people who take it need close monitoring by a dermatologist because of the possibility of severe side effects. Isotretinoin is associated with severe birth defects, so it can't be taken by pregnant women or women who may become pregnant during the course of treatment or within several weeks of concluding treatment. In fact, the drug carries such serious potential side effects that women of reproductive age must participate in a Food and Drug Administration-approved monitoring program to receive a prescription for the drug. In addition, isotretinoin may increase the levels of triglycerides and cholesterol in the blood and may increase liver enzyme levels.
- Oral contraceptives. Oral contraceptives, including a combination of norgestimate and ethinyl estradiol (Ortho-Cyclen, Ortho Tri-Cyclen), have been shown to improve acne in women. However, oral contraceptives may cause other side effects that you'll want to discuss with your doctor.
- Laser and light therapy. Laser- and light-based therapies reach the deeper layers of skin without harming the skin's surface. Laser treatment is thought to damage the oil (sebaceous) glands, causing them to produce less oil. Light therapy targets the bacterium that causes acne inflammation. These therapies can also improve skin texture and lessen the appearance of scars, so they may be good treatment choices for people with both active acne and acne scars.
- Cosmetic procedures. Chemical peels and microdermabrasion may be helpful in controlling acne. These cosmetic procedures — which have traditionally been used to lessen the appearance of fine lines, sun damage and minor facial scars — are most effective when used in combination with other acne treatments.
Doctors may be able to use certain procedures to diminish scars left by acne. These include fillers, dermabrasion, intense light therapy and laser resurfacing.
- Soft tissue fillers. Collagen or fat can be injected under the skin and into scars to fill out or stretch the skin, making the scars less noticeable. Results from this acne scar treatment are temporary, so you'd need to repeat the injections periodically.
- Dermabrasion. Usually reserved for more severe scarring, dermabrasion involves removing the top layer of skin with a rapidly rotating wire brush. Surface scars may be completely removed and deeper acne scars may appear less noticeable. Dermabrasion may cause pigmentation changes for people with darker skin.
- Microdermabrasion. This newer acne scar treatment involves a hand-held device that blows crystals onto skin. These crystals gently abrade or "polish" the skin's surface. Then, a vacuum tube removes the crystals and skin cells. Because just the surface cells are removed, the skin isn't damaged. However, results are subtle and scars may still be noticeable, even after several sessions.
- Laser, light source and radiofrequency treatments. In laser resurfacing, a laser beam destroys the outer layer of skin (epidermis) and heats the underlying skin (dermis). As the wound heals, new skin forms. Less intense lasers (nonablative lasers), pulsed light sources and radiofrequency devices don't injure the epidermis. These treatments heat the dermis and cause new skin formation. After several treatments, acne scars may appear less noticeable. This means shorter recovery times, but treatment typically needs to be repeated more often and results are subtle.
- Skin surgery. A minor procedure (punch excision) cuts out individual acne scars. Stitches or a skin graft repairs the hole left at the scar site.
Prevention
Once your acne improves or clears, you may need to continue your acne medication or other treatment to prevent new acne breakouts. In some cases, you might need to use a topical medication on acne-prone areas, continue taking oral contraceptives or attend ongoing light therapy sessions to keep your skin clear. Talk to your doctor about how you can prevent new eruptions.
You can also prevent new acne breakouts with self-care measures, such as washing your skin with a gentle cleanser and avoiding touching or picking at the problem areas. Other acne prevention tips include:
- Wash acne-prone areas only twice a day. Washing removes excess oil and dead skin cells. But too much washing can irritate the skin. Wash areas daily with a gentle cleanser and use oil-free, water-based skin-care products.
- Use an over-the-counter acne cream or gel to help dry excess oil. Look for products containing benzoyl peroxide or salicylic acid as the active ingredient.
- Avoid heavy foundation makeup. Choose powder cosmetics over cream products because they're less irritating.
- Remove makeup before going to bed. Going to sleep with cosmetics on your skin can clog tiny openings of the hair follicles (pores). Also, be sure to throw out old makeup and clean your cosmetic brushes and applicators regularly with soapy water.
- Wear loosefitting clothing. Tightfitting clothing traps heat and moisture and can irritate your skin. Also, whenever possible, avoid tightfitting straps, backpacks, helmets or sports equipment to prevent friction against your skin.
- Shower after exercising or doing strenuous work. Oil and sweat on your skin can trap dirt and bacteria.
You can avoid or control most acne with good basic skin care and the following self-care techniques:
Wash problem areas with a gentle cleanser. Products such as facial scrubs, astringents and masks generally aren't recommended because they tend to irritate skin, which can worsen acne. Excessive washing and scrubbing also can irritate skin. If you tend to develop acne around your hairline, shampoo your hair frequently.
- Try over-the-counter acne lotion to dry excess oil and promote peeling. Look for products containing benzoyl peroxide or salicylic acid as the active ingredient.
- Avoid irritants. You may want to avoid oily or greasy cosmetics, sunscreens, hair-styling products or acne concealers. Use products labeled "water-based" or "noncomedogenic." For some people, the sun worsens acne. Additionally, some acne medications can make you more susceptible to the sun's rays. Check with your doctor to see if your medication is one of these, and if so, stay out of the sun as much as possible and anytime you have to be in the sun, use sunscreen that doesn't clog your pores.
- Watch what touches your face. Keep your hair clean and off your face. Also avoid resting your hands or objects such as telephone receivers on your face. Tight clothing or hats also can pose a problem, especially if you'll be sweating. Sweat, dirt and oils can contribute to acne.
- Don't pick or squeeze blemishes. Picking or squeezing can cause infection or scarring. Most acne will clear up without this kind of intervention. If you need aggressive treatment, see your doctor or dermatologist.